We all know calcium builds strong bones and teeth — but without vitamin D, your body can’t use calcium effectively. Even if you consume enough calcium, low vitamin D levels reduce its absorption. Simply put, vitamin D is the key that unlocks calcium’s full power1.
Let’s understand how this essential nutrient supports bone health and why maintaining its balance is so important.
How Vitamin D Helps in Calcium Absorption
Vitamin D plays a central role in maintaining calcium balance in the blood.
When calcium enters the intestine from food, it can’t pass into the bloodstream on its own. Vitamin D — in its active form, calcitriol (1,25-dihydroxyvitamin D₃) — helps by:

- Increasing calcium absorption in the small intestine
It stimulates the production of calcium-binding proteins that transport calcium through intestinal cells into the bloodstream. - Maintaining blood calcium levels
When calcium intake is low, vitamin D signals the bones to release stored calcium, ensuring critical functions like nerve transmission and muscle contraction continue smoothly. - Enhancing phosphate absorption
Phosphate works with calcium to strengthen bones and teeth — vitamin D ensures both minerals are absorbed efficiently.
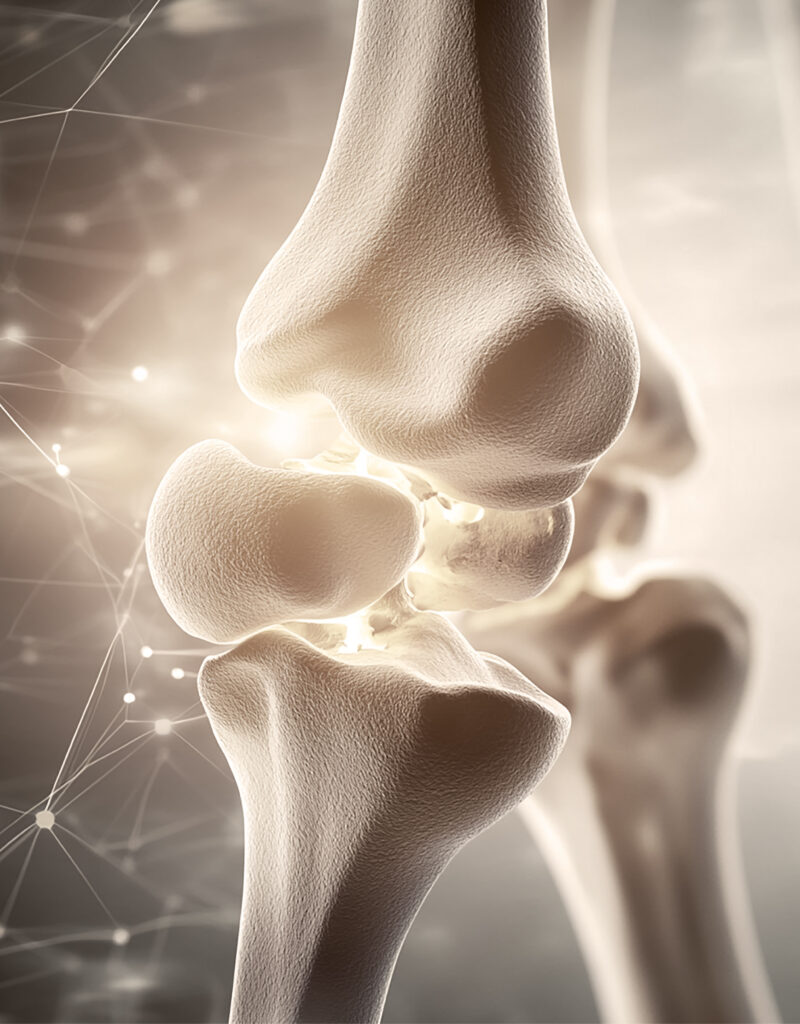
Why Vitamin D is Essential for Bone Health
Calcium and vitamin D work as a team.
If vitamin D is missing, your bones can’t retain calcium, leading to:
- Soft bones in children (rickets)
- Bone pain or muscle weakness in adults (osteomalacia)
- Increased risk of osteoporosis in older adults
Thus, vitamin D ensures that every gram of calcium you take contributes to stronger bones and healthier muscles.
Sources of Vitamin D8
Surprisingly, very few foods naturally contain vitamin D. That’s why it’s often called the “sunshine vitamin.”
Here are the main sources:
Sunlight
- The skin synthesizes vitamin D when exposed to sunlight (UVB rays).
- Around 10–20 minutes of sunlight exposure to arms and face, 3–4 times a week, is generally enough.
- However, factors like sunscreen, skin tone, pollution, and indoor lifestyle can limit this synthesis.

Dietary Sources
- Fatty fish: salmon, mackerel, sardines
- Egg yolks
- Fortified milk, cereals, and plant-based beverages
- Cod liver oil
Supplements
If sunlight and diet aren’t enough, vitamin D supplements (D₂ or D₃) may be prescribed — but always under medical supervision.
Signs of Vitamin D Deficiency
Low vitamin D levels can be subtle but damaging over time. Watch out for:
- Frequent fatigue and low energy
- Bone or joint pain
- Muscle weakness
- Mood swings or depression
- Frequent infections due to weak immunity
The Calcium–Vitamin D Connection in Summary
|
Function |
Role of Calcium |
Role of Vitamin D |
|---|---|---|
|
Bone Strength |
Builds and maintains bone density |
Helps calcium reach and stay in bones |
|
Muscle Function |
Enables contraction |
Facilitates calcium entry into muscle cells |
|
Nervous System |
Supports signal transmission |
Ensures calcium balance for nerve function |
They’re interdependent — calcium builds the structure, and vitamin D makes sure it gets there!
Final Thoughts
Vitamin D may seem like a small nutrient, but it’s a powerful regulator of calcium and bone metabolism. Without it, even a calcium-rich diet won’t fully protect you from bone loss or muscle weakness.
So next time you step out into the sun, remember — you’re not just soaking in warmth; you’re building your bones.
A few rays of sunlight + balanced diet = stronger bones, better immunity, and healthier you!
References
- Heaney, R. P. Vitamin D Depletion and Effective Calcium Absorption. Journal of Bone and Mineral Research 18, 1342–1342 (2003).
- Jiang, H. et al. Targeting 1,25(OH)2D-mediated calcium absorption machinery in proximal colon with calcitriol glycosides and glucuronides. J Steroid Biochem Mol Biol 198, 105574 (2020).
- Fleet, J. C. The role of vitamin D in the endocrinology controlling calcium homeostasis. Mol Cell Endocrinol 453, 36–45 (2017).
- Fukumoto, S. Phosphate metabolism and vitamin D. Bonekey Rep 3, (2014).
- Sahay, M. & Sahay, R. Rickets-vitamin D deficiency and dependency. Indian J Endocrinol Metab 16, 164 (2012).
- Minisola, S. et al. Osteomalacia and Vitamin D Status: A Clinical Update 2020. JBMR Plus 5, (2021).
- Johnston, C. B. & Dagar, M. Osteoporosis in Older Adults. Medical Clinics of North America 104, 873–884 (2020).
- Lamberg-Allardt, C. Vitamin D in foods and as supplements. Prog Biophys Mol Biol 92, 33–38 (2006).